Vital Signs
Vital signs include the measurement of: temperature, respiratory rate, pulse, blood pressure and, where appropriate, blood oxygen saturation. These numbers provide critical information (hence the name "vital") about a patient's state of health. In particular, they:
- Can identify the existence of an acute medical problem.
- Are a means of rapidly quantifying the magnitude of an illness and how well the body is coping with the resultant physiologic stress. The more deranged the vitals, the sicker the patient.
- Are a marker of chronic disease states (e.g. hypertension is defined as chronically elevated blood pressure).
Most patients will have had their vital signs measured by an RN or health care assistant before you have a chance to see them. However, these values are of such great importance that you should get in the habit of repeating them yourself, particularly if you are going to use these values as the basis for management decisions. This not only allows you to practice obtaining vital signs but provides an opportunity to verify their accuracy. As noted below, there is significant potential for measurement error, so repeat determinations can provide critical information.
Getting Started: The examination room should be quiet, warm and well lit. After you have finished interviewing the patient, provide them with a gown (a.k.a. "Johnny") and leave the room (or draw a separating curtain) while they change. Instruct them to remove all of their clothing (except for briefs) and put on the gown so that the opening is in the rear. Occasionally, patient's will end up using them as ponchos, capes or in other creative ways. While this may make for a more attractive ensemble it will also, unfortunately, interfere with your ability to perform an examination! Prior to measuring vital signs, the patient should have had the opportunity to sit for approximately five minutes so that the values are not affected by the exertion required to walk to the exam room. All measurements are made while the patient is seated.
Observation: Before diving in, take a minute or so to look at the patient in their entirety, making your observations, if possible, from an out-of-the way perch. Does the patient seem anxious, in pain, upset? What about their dress and hygiene? Remember, the exam begins as soon as you lay eyes on the patient.
Temperature: This is generally obtained using an oral thermometer that provides a digital reading when the sensor is placed under the patient's tongue. As most exam rooms do not have thermometers, it is not necessary to repeat this measurement unless, of course, the recorded value seems discordant with the patient's clinical condition (e.g. they feel hot but reportedly have no fever or vice versa). Depending on the bias of a particular institution, temperature is measured in either Celcius or Farenheit, with a fever defined as greater than 38-38.5 C or 101-101.5 F. Rectal temperatures, which most closely reflect internal or core values, are approximately 1 degree F higher than those obtained orally.
Respiratory Rate: Respirations are recorded as breaths per minute. They should be counted for at least 30 seconds as the total number of breaths in a 15 second period is rather small and any miscounting can result in rather large errors when multiplied by 4. Try to do this as surreptitiously as possible so that the patient does not consciously alter their rate of breathing. This can be done by observing the rise and fall of the patient's hospital gown while you appear to be taking their pulse. Normal is between 12 and 20. In general, this measurement offers no relevant information for the routine examination. However, particularly in the setting of cardio-pulmonary illness, it can be a very reliable marker of disease activity.
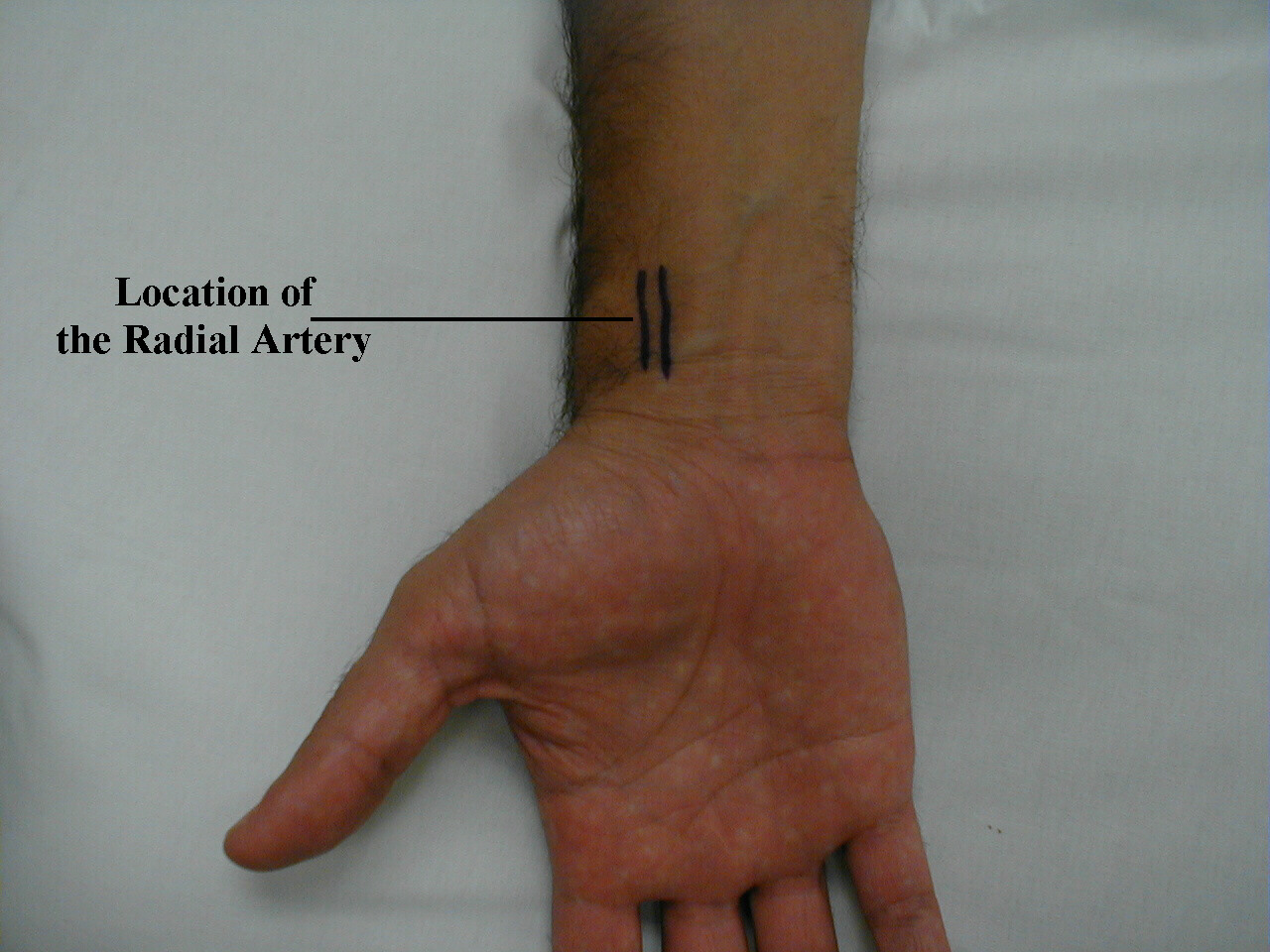
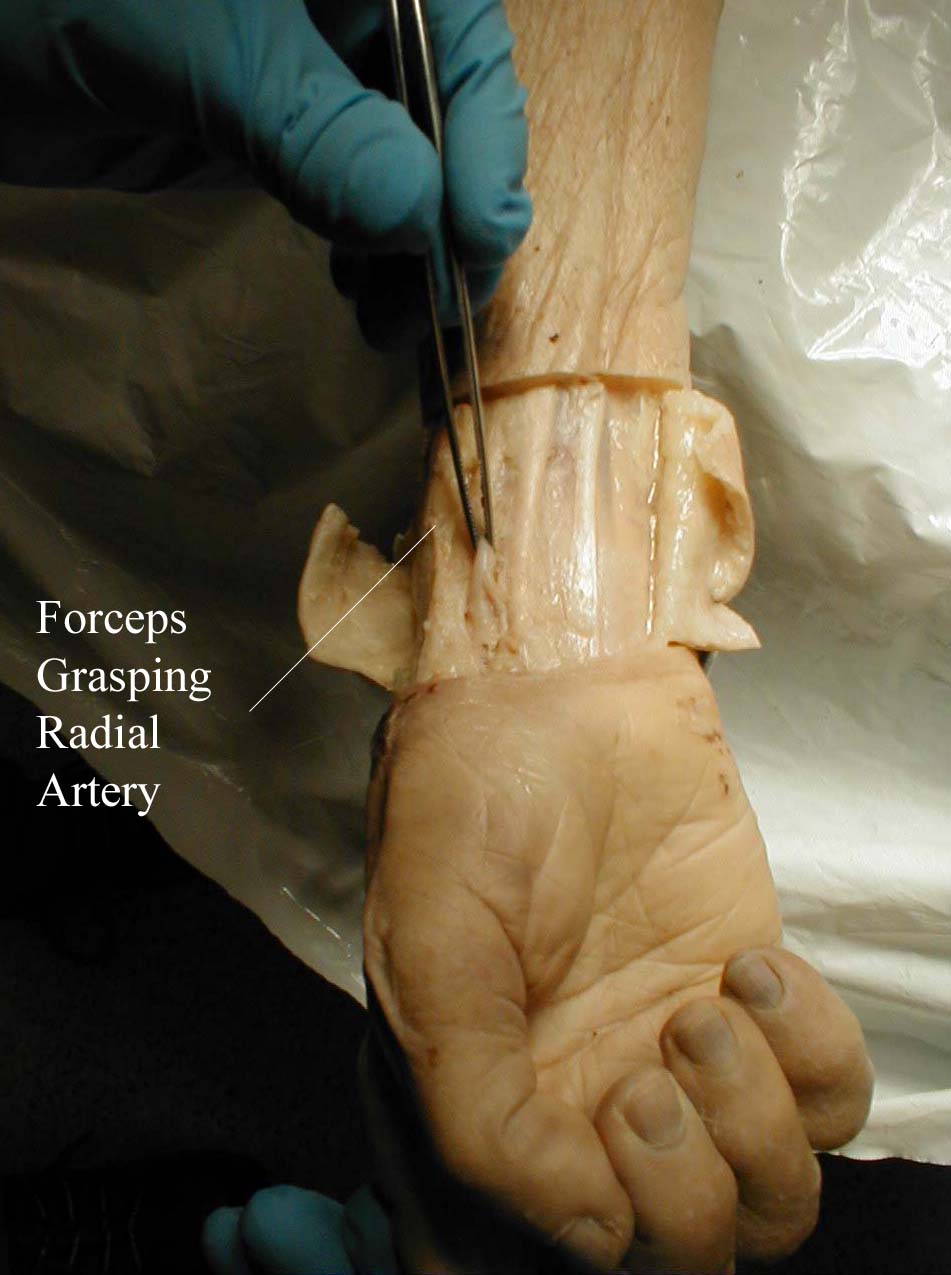
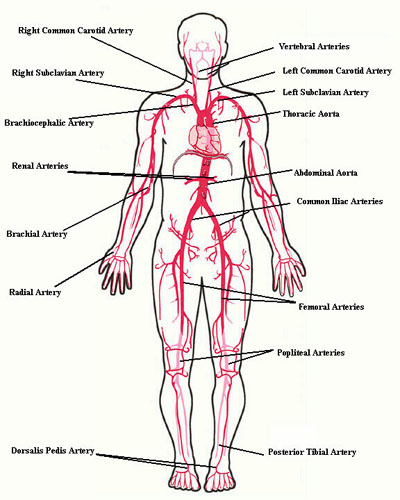
Pulse: This can be measured at any place where there is a large artery (e.g. carotid, femoral, or simply by listening over the heart), though for the sake of convenience it is generally done by palpating the radial impulse. You may find it helpful to feel both radial arteries simultaneously, doubling the sensory input and helping to insure the accuracy of your measurements. Place the tips of your index and middle fingers just proximal to the patients wrist on the thumb side, orienting them so that they are both over the length of the vessel.
Frequently, you can see transmitted pulsations on careful visual inspection of this region, which may help in locating this artery. Upper extremity peripheral vascular disease is relatively uncommon, so the radial artery should be readily palpable in most patients. Push lightly at first, adding pressure if there is a lot of subcutaneous fat or you are unable to detect a pulse. If you push too hard, you might occlude the vessel and mistake your own pulse for that of the patient. During palpation, note the following:
- Quantity: Measure the rate of the pulse (recorded in beats per minute). Count for 30 seconds and multiply by 2 (or 15 seconds x 4). If the rate is particularly slow or fast, it is probably best to measure for a full 60 seconds in order to minimize the impact of any error in recording over shorter periods of time. Normal is between 60 and 100.
- Regularity: Is the time between beats constant? In the normal setting, the heart rate should appear metronomic. Irregular rhythms, however, are quite common. If the pattern is entirely chaotic with no discernable pattern, it is referred to as irregularly irregular and likely represents atrial fibrillation. Extra beats can also be added into the normal pattern, in which case the rhythm is described as regularly irregular. This may occur, for example, when impulses originating from the ventricle are interposed at regular junctures on the normal rhythm. If the pulse is irregular, it's a good idea to verify the rate by listening over the heart (see cardiac exam section). This is because certain rhythm disturbances do not allow adequate ventricular filling with each beat. The resultant systole may generate a rather small stroke volume whose impulse is not palpable in the periphery.
- Volume: Does the pulse volume (i.e. the subjective sense of fullness) feel normal? This reflects changes in stroke volume. In the setting of hypovolemia, for example, the pulse volume is relatively low (aka weak or thready). There may even be beat to beat variation in the volume, occurring occasionally with systolic heart failure.
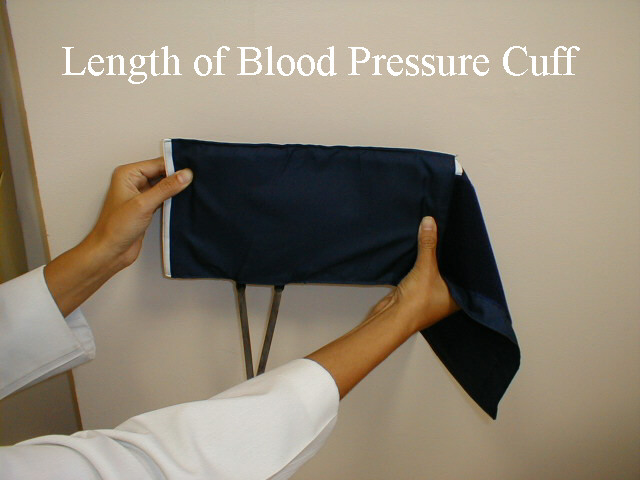
Blood Pressure: Blood pressure (BP) is typically measured using an anaeroid manometer, with readings reported in millimeters of mercury (mm Hg). While most BP readings in hospitals and clinics are initially taken with digital machines, it's still relevant to learn how to use manual cuffs, as clinicians will need to check the validity of digital readings on occasion (e.g. when BP unexpectedly high or low). The size of the BP cuff will affect the accuracy of these readings. The inflatable bladder, which can be felt through the vinyl covering of the cuff, should reach roughly 80% around the circumference of the arm while its width should cover roughly 40%. If it is too small, the readings will be artificially elevated. The opposite occurs if the cuff is too large. Clinics should have at least 2 cuff sizes available, normal and large. Try to use the one that is most appropriate, recognizing that there will rarely be a perfect fit.

In order to measure the BP, proceed as follows:
- The patient should be seated, ideally resting for 5 minutes prior to measuring
their blood pressure. Legs should be uncrossed, feet placed flat on the floor.
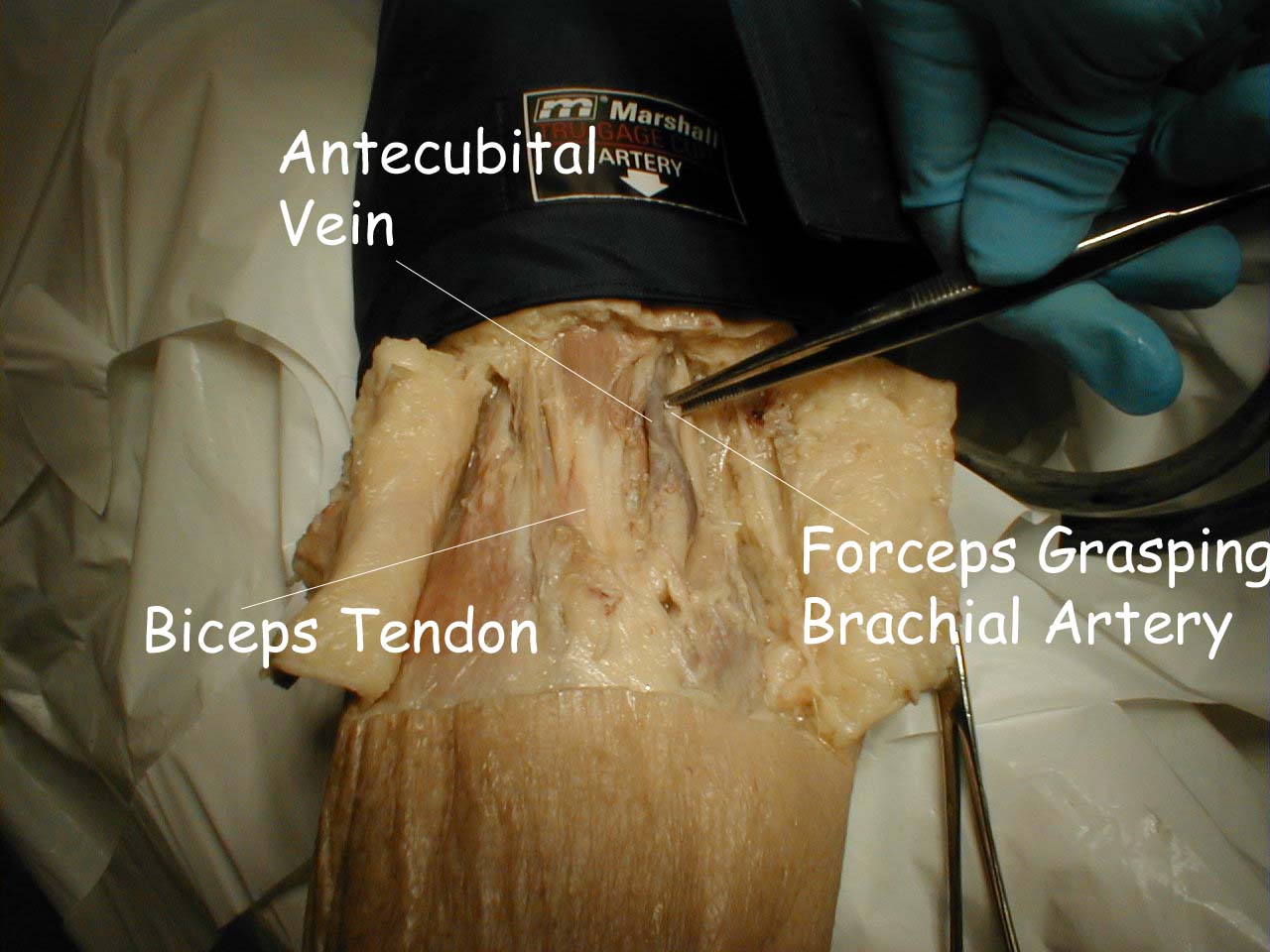
Antecubital Fossa
The pictures below demonstrate the antecubital fossa anatomy (surface anatomy on the left, gross anatomy on the right).

- The cuff should be placed directly on the skin (i.e. do not put it over
clothes). Sliding a loose fitting t-shirt up so that the skin is exposed is
fine. However, try not to roll tight fitting shirts up over the bicep. In that
setting, it’s better to have the patient take their shirt off (using a gown to
keep the rest of their body covered).
- Wrap the cuff around the patient's upper arm so that the line marked "artery" is roughly over the brachial artery, located towards the medial aspect of the antecubital fossa (i.e. the crook on the inside of their elbow). The placement does not have to be exact nor do you actually need to identify this artery by palpation.
- Turn the valve on the pumping bulb clockwise (may be counter clockwise in some cuffs) until it no longer moves. This is the position which allows air to enter and remain in the bladder.
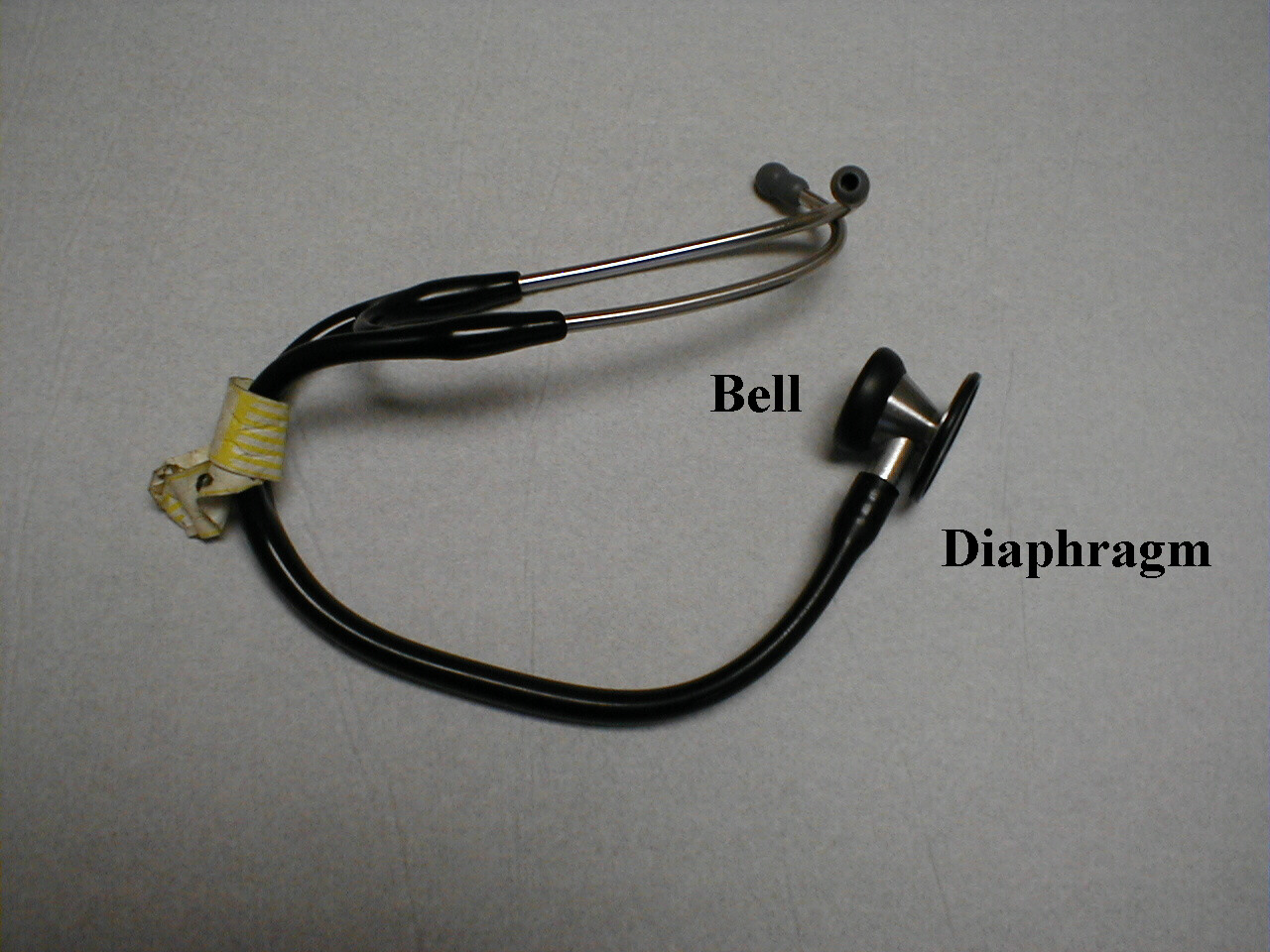
- Hold the bell in place with your left hand. Use your right hand to pump the bulb until you have generated 150 mmHg on the manometer. This is a bit above the top end of normal for systolic blood pressure (SBP). Then listen. If you immediately hear sound, you have underestimated the SBP. Pump up an additional 20 mmHg and repeat. Now slowly deflate the blood pressure cuff (i.e. a few mm Hg per second) by turning the valve in a counter-clockwise direction while listening over the brachial artery and watching the pressure gauge. The first sound that you hear reflects the flow of blood through the no longer completely occluded brachial artery. The value on the manometer at this moment is the SBP. Note that although the needle may oscillate prior to this time, it is the sound of blood flow that indicates the SBP.
- Continue listening while you slowly deflate the cuff. The diastolic blood
pressure (DBP) is measured when the sound completely disappears. This is the
point when the pressure within the vessel is greater then that supplied by
the cuff, allowing the free flow of blood without turbulence and thus no audible
sound. These are known as the Sounds of Korotkoff.
Technique for Measuring Blood Pressure

- Repeat the measurement on the patient's other arm, reversing the position of your hands. The two readings should be within 10-15 mm Hg of each other. Differences greater than this imply that there is differential blood flow to each arm, which most frequently occurs in the setting of subclavian artery atherosclerosis.
- Occasionally you will be unsure as to the point where systole or diastole occurred and wish to repeat the measurement. Ideally, you should allow the cuff to completely deflate, permit any venous congestion in the arm to resolve (which otherwise may lead to inaccurate measurements), and then repeat a minute or so later. Furthermore, while no one has ever lost a limb secondary to BP cuff induced ischemia, repeated measurement can be uncomfortable for the patient, another good reason for giving the arm a break.
- Avoid moving your hands or the head of the stethescope while you are taking readings as this may produce noise that can obscure the Sounds of Koratkoff.
- You can verify the SBP by palpation. To do this, position the patient's right arm as described above. Place the index and middle fingers of your right hand over the radial artery. Inflate the cuff until you can no longer feel the pulse, or simply to a value 10 points above the SBP as determined by auscultation. Slowly deflate the cuff until you can again detect a radial pulse and note the reading on the manometer. This is the SBP and should be the same as the value determined with the use of your stethescope.
Implications, interpretation and other clinical pearls related to hypertension:
Hypertension is a common disease, affecting > 40% of the adult US population. With the steady increase in obesity rates, it’s anticipated that this % will continue to increase.
Normal values and definitions for hypertension are as follows:
- Normal < 120/80 mm Hg
- Elevated: SBP 120-129 and DBP < 80 mm Hg
- Stage I hypertension: SBP 130-39 or DBP 80-89 mm Hg
- Stage II hypertension: SBP >= 140 or DBP >= 90 mm Hg
The diagnosis of hypertension is typically based on 2 readings, done at 2 different settings. A one-time measurement > 160/100 should prompt consideration for treatment. Home readings (with a validated device) can also be used for the diagnosis and management of hypertension. Careful attention must be paid to the use of appropriate techniques (described above), as measurement error(s) can lead to inaccurate values and diagnoses.
Hypertension (HTN) causes and accelerates the progression of: Coronary artery disease, heart failure with reduced ejection fraction (HFrEF), heart failure with preserved ejection fraction (HFpEF), left ventricular hypertrophy, aortic aneurysm development, peripheral arterial disease, stroke, chronic kidney disease, and retinopathy. The risk of HTN induced damage correlates with both the height of BP and the chronicity of elevation (i.e. longer and higher is worse).
The treatment of HTN prior to the development of Target Organ Damage (a.k.a. TOD) is referred to as "primary prevention," while treatment to prevent and/or slow progression once disease has already been established is called "secondary prevention." Evaluation of patients with HTN requires careful history taking, physical exam, labs, and other studies to search for co-morbid problems (e.g. diabetes, sleep apnea, etc.) and/or occult TOD. Most patients with HTN are asymptomatic, at least until they develop target organ damage, which can take years to manifest.
A few additional clinically oriented thoughts:
- The development of hypertension is directly affected by weight, inactivity, alcohol consumption, and salt intake. As such, life style interventions directed to address each of these issues are important. Making use of resources and persons with expertise in these areas can increase the effectiveness of interventions. This can include enlisting the help of nutritionists, exercise programs, comprehensive weight loss systems, alcohol/addiction specialists, etc. And it’s important for clinicians to continually assess every patient’s interest (e.g. via motivational interviewing techniques) and level of engagement at each interaction with the health care system. Lifestyle interventions alone are reasonable for patients with stage I hypertension and < 10% risk (Estimated by ACC Atherosclerotic Risk Calculator or other similar tool). And even if meds are ultimately used, lifestyle changes can have a synergistic effect.
- Hypertension swims in the same vascular risk factor waters as diabetes, hyperlipidemia, and smoking. As such, these other areas must also be addressed, including appropriate use of aspirin.
- The trigger value at which anti-hypertensive treatments should be initiated varies with a patient’s risk for atherosclerosis. In those with established disease (e.g. known coronary artery disease, Diabetes), or 10y risk (Estimated by ACC Atherosclerotic Risk Calculator or other similar tool) > 10%, pharmacologic treatment is started if BP > 130/80. For those without known disease and risk < 10%, medications should be initiated if BP> 140/90. It’s also worth noting that BP targets and thresholds to initiate treatment have changed over the years and will likely continue to do so.
- For those receiving treatment, BP target is < 130/80, regardless of ASCVD risk.
- Most drugs within the same class (e.g. any of the 8 or so ACE-Inhibitors) are equally efficacious.
- Effective treatment requires continual reassessment of medication adherence - a major reason for lack of response to Rx. It helps to know the common side effects for each medication, as they can affect adherence (e.g. ACE-I →cough; thiazides → mild increase in urination; all anti-hypertensive meds→ hypotension).
- The majority of patients with HTN (> 60%) will require at least 2 meds for treatment.
- Initial medication choices can be thiazide diuretics, Ace- Inhibitors/Angiotensin Receptor Blockers, or calcium channel blockers.
- For those with starting BP values > 160/100, it's best to start with 2 meds simultaneously. Instances where 3 or more medications are required is relatively common, often related to obesity and other comorbid conditions (e.g. CKD). Non-adherence should also be considered.
- Certain conditions favor particular meds, including: Diabetes → ACE-I or ARBs; Coronary artery disease → Beta blockers; HFrEF→ Ace-I/ARBs, selective Beta blockers, loop diuretics.
- Where you start isn't where you end, so expect to reassess BP and related issues repeatedly over time. This includes review of adherence to medication and other treatment plans, weight gain, use of medications with adverse affect on BP (e.g. NSAIDs, ADHD meds), and the appearance of new symptoms (e.g. SOB, CP) that might suggest hypertension related TOD.
- Most patients with elevated blood pressure suffer from primary
hypertension (i.e. the elevation in blood pressure is the primary
disorder). Secondary hypertension (elevation in BP secondary to another,
treatable condition) is much less common - though worth thinking about
in the right situation. Secondary causes should be considered in young
patients (e.g. < 30), those with refractory hypertension (requiring 3 or more meds), new
onset hypertension age> 65, accelerated hypertension
and in the setting of specific clinical clues. Causes of secondary
hypertension, along with suggestive features, include the following:
- Medications (e.g. NSAIDs, decongestants, stimulants, many others) or excess alcohol intake.
- Chronic kidney disease: As evidenced by decreased GFR on labs and symptoms such as SOB, fatigue; PE: Hypertension, edema if volume overload.
- Obstructive sleep apnea: Poorly rested in the morning, awakening in middle of night gasping for air, snoring, noted by partner to stop breathing, chronic day time sleepiness; PE: Elevated BMI, difficulty visualizing the posterior pharynx, large neck diameter (> 17 inches men, > 16 inches women).
- Hyperaldosteronism: Unexplained hypokalemia and/or hypokalemia that is disproportionate to inciting medications; PE: Hypertension.
- Hypothyroidism: Weight gain, constipation, fatigue, weakness, dry skin, cold intolerance; PE: Hypertension pretibial edema, lateral thinning of eyebrows, decreased relaxation phase of reflexes, sometimes thyromegaly.
- Hyperthyroidism: Weight loss, diarrhea, fatigue, weakness, irritability, heat intolerance, palpitations; PE: elevated heart rate (atrial fibrillation), hypertension, tremor, proptosis, hyper-reflexia, warm/moist skin.
- Renal artery stenosis: Chronic kidney disease; PE: Hypertension, sometimes abdominal bruit, decreased peripheral pulses/other evidence atherosclerosis.
- Pheochromocytoma: Paroxysms of hypertension, awareness of heart pounding, headache, fatigue; PE: Hypertension, sweating, elevated heart rate during a “spell”
- Excess cortisol production (Cushings): Central weight gain, weakness, fatigue, bruising; PE: Hypertension, obesity, posterior cervical fat pad (“buffalo hump”), abdominal striae, round face (‘moon facies’), echymoses.
- Growth hormone excess (Acromegaly): Growth of hands and feet as an adult, fatigue, weakness, joint pain, headache, altered vision; PE: Hypertension, large jaw, gaps between teeth, prominent brow, large hands and feet, large tongue, bi-temporal visual field cuts.
- Coarctation of the aorta: Typically noted in young (< 30 y.o.) patients; PE: Hypertension, BP difference between arms and legs, diminished peripheral pulses (i.e. femoral compared with radial), bruit (back, chest, or abdomen).
- Acute interventions to immediately lower BP are usually reserved for those instances when there is clear evidence of acute symptoms related to acute TOD, referred to as a hypertensive emergency. Those situations include acute heart failure, coronary ischemia, hypertensive encephalopathy, and acute kidney injury.
- Low end of normal BP is ~ 90/100/70, though the minimal blood pressure required to maintain perfusion varies with the individual patient. Therefore, interpretation of low values must take into account the clinical situation. Those with poorly functioning hearts, for example, can adjust to a chronically low SBP (e.g. 80-90) and live without symptoms of hypo-perfusion. However others, used to higher baseline values, might become quite ill if their SBPs were suddenly decreased to these same levels.
Orthostatic (a.k.a. postural) measurements of pulse and blood pressure are often part of the assessment for hypovolemia and/or dizziness. This requires first measuring HR and BP when the patient is supine and then repeating them after the patient has stood for a few minutes.
Normally, SBP doesn’t vary by more than ~20 points and DBP by more than ~10 points when a patient moves from lying to standing. In the setting of significant volume depletion, a greater drop may be seen. This may also be associated with symptoms of cerebral hypo-perfusion (e.g. light headedness). In the setting of acute GI bleeding, for example, a drop in blood pressure and/or rise in heart rate when moving from lying to standing is a marker of significant blood loss and has important prognostic implications. It is also possible to have volume loss without attendant postural changes (i.e. the absence of changes doesn’t rule out hypovolemia).
Orthostatic measurements may also be used to determine if postural dizziness or syncope/presyncope are the result of a fall in blood pressure. For example, patients who suffer from diabetes may have autonomic nervous system dysfunction and impaired ability to appropriately vasoconstrict when changing positions. If their dizziness/lightheadedness is the result of orthostatic changes, then their BP will drop when they move from a lying to standing position and their symptoms will be reproduced. The 20-point value is a rough guideline. In general, the greater the change in BP, the more likely it is to cause symptoms and be of clinical significance.
The following are links to useful additional information about BP measurement and hypertension.
- AHA/ACC 2017 Guideline for High Blood Pressure in Adults
- New England Journal of Medicine - BP Measurement
- Moser M, et al. Resistant or difficult to control hypertension. NEJM 2006; 355: 385-92.
Oxygen Saturation: Over the past decade, this non-invasive measurement of gas exchange and red blood cell oxygen carrying capacity has become available in all hospitals and many clinics. While imperfect, it can provide important information about cardio-pulmonary dysfunction and is considered by many to be a fifth vital sign. In particular, for those suffering from either acute or chronic cardio-pulmonary disorders, it can help quantify the degree of impairment.