Musculo-Skeletal Examination
Low Back Pain
Low back pain is a very common condition. Examination and history provide important clues as to its etiology.
For Additional Information See: Digital DDx: Low Back Pain
Function and Anatomy:
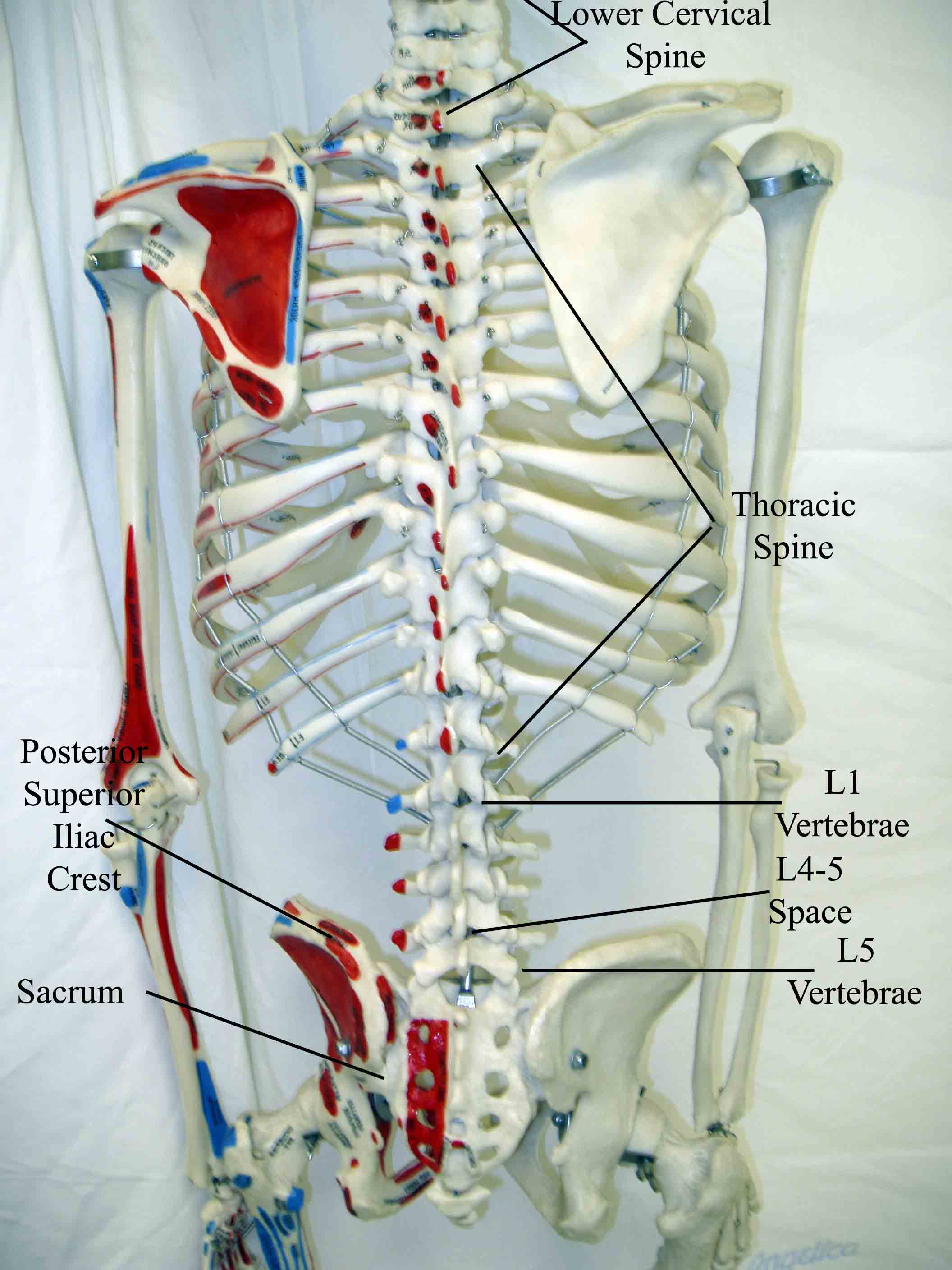
The lumbar spine must support a tremendous amount of weight, protect the spinal
cord and yet still maintain flexibility that maintains range of motion. The low
back is formed by 5 lumbar vertebrae and the sacrum. Each vertebrae articulates
with the one above and below it in a precise fashion that helps to maximize function.
The bones are covered by periosteum, which is innervated and thus generates pain
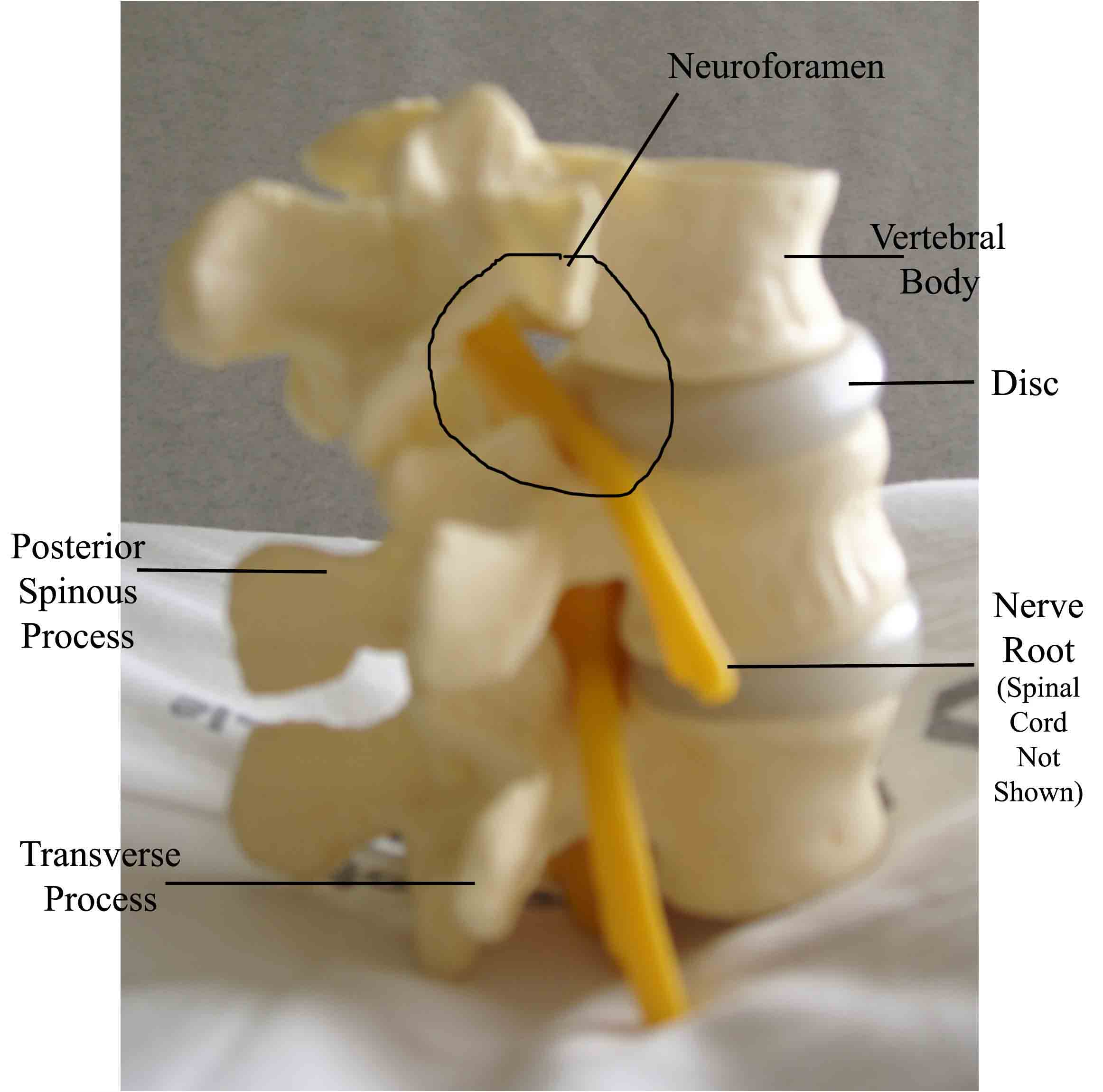
if inflamed (see below). The vertebrae are separated by discs, which allow for
smooth, cushioned articulation. The outer aspect of the disc is made of a tough
fibrous tissue called the annulus fibrosis, while the inner aspect is gelatinous
and known as the nucleus propulsus. Powerful ligaments connect the verterbrae
to each other along their anterior and posterior aspects. The spinal cord runs
in a bony canal, just posterior to the main body of the vertebrae. This space
is well designed to protect the delicate nervous tissue of the cord. The vertebral
column has regularly spaced lateral openings known as neuroforamina, through which
nerve roots exit and travel to the target organs which they innervate. The actual
cord ends at about the L1 level. Below this point, nerve roots (known as the cauda
equine) drape down and fill the lower aspect of the spinal canal. The neuro formaina
are identified by the vertebrae that are above and below it (e.g L5-S1 neuro foramen
sits between the L5 and S1 vertebrae). Spinous processes make up the most posterior
aspect of the spinal column and are palpable on exam. The rest of the structures
(e.g. discs, spinal cord, nerve roots) are not palpable. In terms of surface landmarks,
it's helpful to identify the posterior
superior iliac crest. This point is roughly on line with the L4-5 intervertebral space.
Review of Spinal Anatomy.
Common Benign Pain Syndromes--Symptoms and Etiology:
- Non-specific musculoskeletal pain: This is the most common cause of back pain. Patients present with lumbar area pain that does not radiate, is worse with activity, and improves with rest. There may or may not be a clear history of antecedent over use or increased activity. The pain is presumably caused by irritation of the paraspinal muscles, ligaments or vertebral body articulations. However, a precise etiology is difficulty to identify.
- Radicular Symptoms:
Often referred to as "sciatica," this is a pain syndrome caused by
irritation
of one of the nerve roots as it exits the spinal column. The root
can become inflamed
as a result of a compromised neuroforamina (e.g. bony osteophyte
that limits size
of the opening) or a herniated disc (the fibrosis tears, allowing
the propulsus
to squeeze out and push on the adjacent root). Sometimes, it's not
precisely clear
what has lead to the irritation. In any case, patient's report a
burning/electric
shock type pain that starts in the low back, traveling down the
buttocks and along
the back of the leg, radiating below the knee. Symptoms and exam
findings for lumbar and sacral root pathology are described below.
Of note, L5 and S1 are the most commonly affected roots.
- L2 root dysfunction: Pain radiates from the low back to the upper leg. If there are sensory deficits, they will affect the lateral and anterior upper thigh. If there is weakness, it will affect the quadriceps (knee extension) and psoas (hip flexion) muscles.
- L3 root dysfunction: Pain radiates from the low back to upper leg. If there are sensory deficits, they will affect the lower medial thigh. If there is weakness, it will affect the quadriceps (knee extension) and psoas (hip flexion) muscles. If reflexes are affected, the patellar will be impaired.
- L4 root dysfunction: Pain radiates from the low back to below the knee. If there are sensory deficits, they will affect the medial aspect of the lower leg. If there is weakness, it will affect the quadriceps (knee extension) muscle. If reflexes are affected, the patellar will be impaired.
- L5 root dysfunction: Pain radiates from the low back to below the knee. If there are sensory deficits, they will cause numbness on the top of the foot. If there is weakness, it will affect foot inversion and great toe extension.
- S1 root dysfunction: Pain radiates from the low back to below the knee. If there are sensory deficits, they will affect the lateral aspect of foot. If there is weakness, it will cause impaired plantar flexion. If relexes are affected, the achilles will be impaired.
- Lumbar Spinal Stenosis: Pain starts in the low back and radiates down the buttocks bilaterally, continuing along the backs of both legs. Symptoms are usually worse with walking and improve when the patient bends forward. Patient's may describe that they relieve symptoms by leaning forward on their shopping carts when walking in a super market. This is caused by spinal stenosis, a narrowing of the central canal that holds the spinal cord. The limited amount of space puts pressure on the nerve roots when the patient walks, causing the symptoms (referred to as neurogenic claudication). Spinal stenosis can be congenital or develop over years as a result of djd of the spine. As opposed to true claudication (pain in calfs/lower legs due to arterial insufficiency), pain resolves very quickly when person stops walking and assumes upright position. Also, peripheral pulses should be normal.
- Mixed symptoms: In some patients, more then one process may co-exist, causing elements of more then one symptom syndrome to co-exist.
Red Flags:
There are a variety of ominous processes that cause low back pain, particularly in older patients (> 50). These problems carry significant morbidity and mortality and mandate a focused and rapid evaluation (including lab and imaging studies) different from what is required for the relatively benign processes described above. Careful history taking and examination can help distinguish these problems. Historical keys include:
- Pain that doesn't get better when lying down/resting.
- Pain associated by systemic symptoms of inflammation (e.g. fever, chills), in particular in those at risk for systemic infection that could seed the spinal area (e.g. IV drug users, patients with bacteremia).
- Known history of cancer, in particular malignancies that metastasize to bone (e.g. prostate, breast, lung).
- Trauma, particularly if of substantial force.
- Osteoporosis, which increases risk of compression fracture (vertebrae collapsing under the weight they must bear). More common as people age, women > men.
- Anything suggesting neurological compromise. In particular, weakness in legs suggesting motor dysfunction. Also, bowel or bladder incontinence, implying diffuse sacral root dysfunction. Note: it can sometimes be difficult to distinguish true weakness from motor limitation caused by pain.
- Pain referred to the back from other areas of the body (e.g. intra-abdominal or retroperitoneal processes). Could include: Pyelonephritis, leaking/rupturing abdominal aortic aneurysm, posterior duodenal ulcer, pancreatitis, etc.
Examination Keys:
- Vital signs. In particular, pain may be reflected by increase pulse, BP or pain score (if asked). Also, temperature if concern re an infectious process.
- Observe gait. Is it slow, limited by pain?
- Look at the lumbar spine area. Any skin abnormalities suggesting underlying inflammation? Normal curvature is as follows: Cervical spine sweeps anteriorly, thoracic spine sweeps posteriorly, and lumbro-sacral spine sweeps anteriorly.
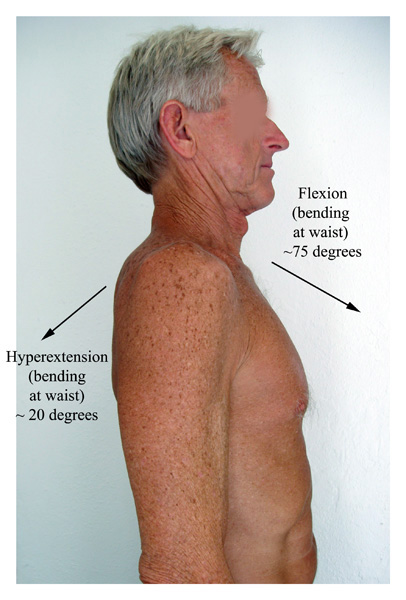
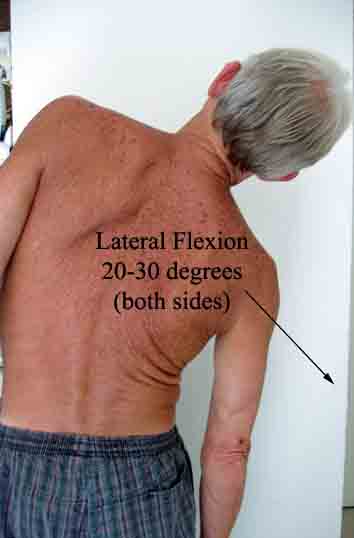
- Range of motion testing should include forward flexion,
hyperextension,
lateral flexion, and rotation.
- Can the patient point to the precise area of the pain? Is it along the vertebral column? Para-spinal, as might occur with spasm? Radiating down the legs as would occur with nerve root irritation?
- Palpate the spine. Processes that inflame the bone (e.g.
compression fracture,
osteomyelitis, metastatic disease) will generate pain when the
affected vertebrae
is palpated or percussed.
 Spine Percussion
Spine Percussion - Is the pain in the costo-vertebral angle area, suggestive of a
kidney infection?
 Location of kidneys drawn on back. In the setting of kidney infection
Location of kidneys drawn on back. In the setting of kidney infection
(pyelonephritis), percussion over this area will cause pain. - If the patient's complains of a radiating type pain down one
leg, suggestive
of nerve root irritation, proceed as follows:
- Ask the patient to lie down on their back.
- Have the patient completely relax the affected leg.
- Cup the heel of their foot and gently raise the leg. If
there is nerve
root irritation, the patient will experience their
typical pain when the
leg is elevated between 30 and 60 degrees. This is
referred to at the
"straight leg raise test" and is sensitive for
identifying root pathology
(i.e. if it does not reproduce pain, root irritation
unlikely). Sensitive
(75-90%), but not specific. Therefore, negative test
helps rule out nerve
root irritation as cause of pain. d. If the straight leg
test is positive,
repeat the same test on the opposite leg. This is called
the crossed straight
leg raised test and is 85-95% specific for root
irritation, but not sensitive.
Therefore, positive test makes root irritation the
likely etiology of
the symptoms.
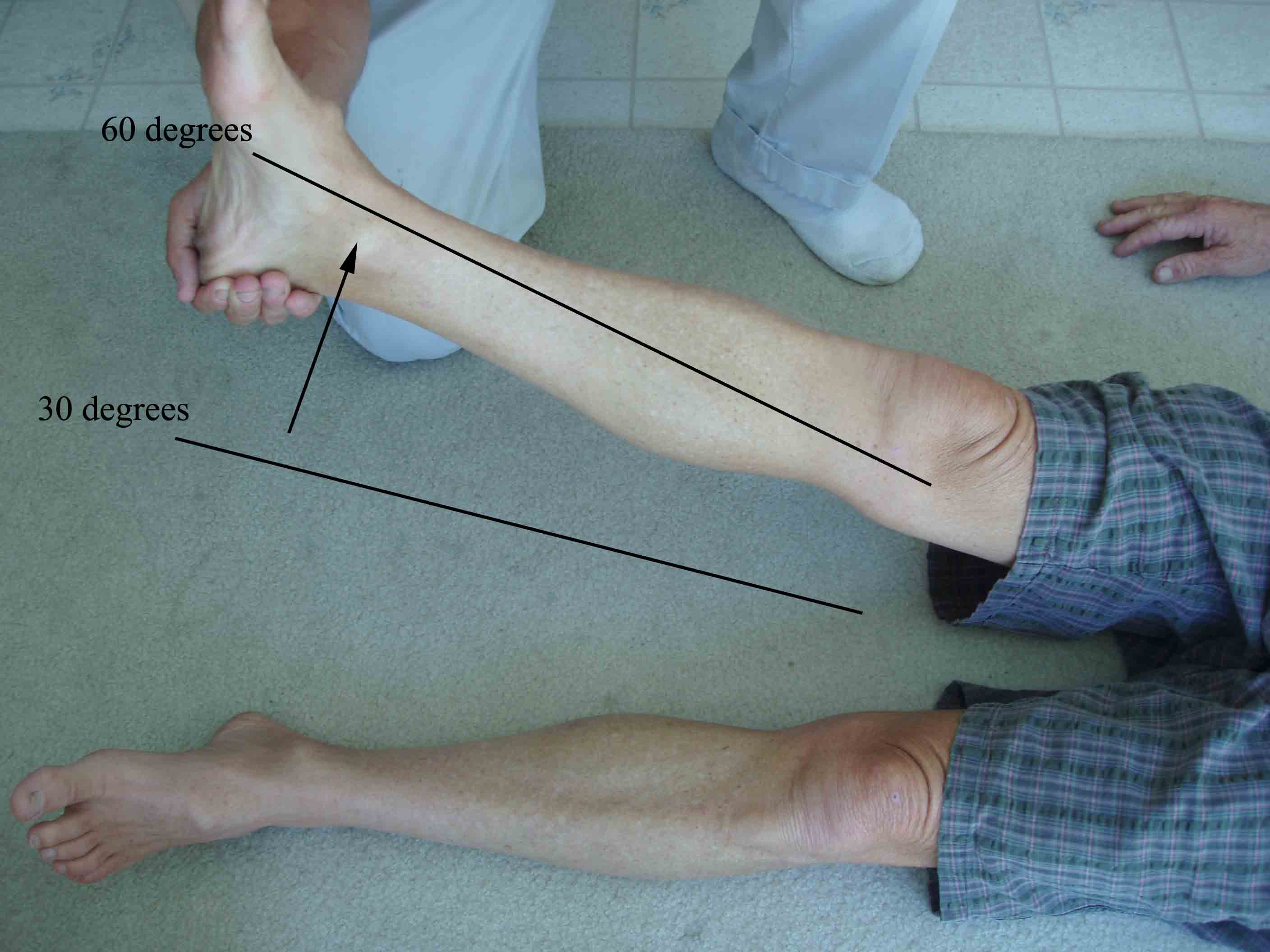 Leg Raise Test
Leg Raise Test
- Assess bilateral lower extremity strength. In particular, if concern that nerve root pathology has lead to motor dysfunction (quite uncommon) check the following: a. Resisted great toe extension (extensor hallicis longus), mediated by the L5 nerve root. b. Walking on toes, as plantar flexion is mediated by the S1 root.
- Reflexes, in particular the Achilles, which is a function of the
S1 root.
Detailed review of neurologic examination. - Distal sensation, paying attention to the L5 and S1 dermatomes.
- If patient's note any bowel or bladder symptoms, assess sacral
nerve root
function as follows:
- Rectal tone: Patient should be able to contract anal sphincter around examining finger when directed to do so.
- Saddle area anesthesia: This is the region around the rectum, genitalia and inner thighs. Patients should be able to easily distinguish light touch and pin prick.
- Post Void Residual: Patient's should normally be able to completely empty their bladders. In acute sacral root dysfunction, this may be compromised. This can be assessed by using either a bedside bladder scan or placement of a foley catheter. While not part of the typical exam, it is important is this setting.
- Gently internally and externally rotate the hip. In pyriformis syndrome internal rotation will stretch an already tight external rotator, causing further compression of the underlying nerve. This should reproduce the patient's symptoms. Straight and crossed leg raising will not reproduce symptoms.
- Check pulses in feet to assure that symptoms not related to
peripheral
vascular disease.
Detailed review of lower extremity examination. - If any concern that symptoms are referred from the abdomen, a detailed exam of this area is performed. Also, if concern that back pain is a manifestation of systemic illness, appropriate detailed general exam should be performed.